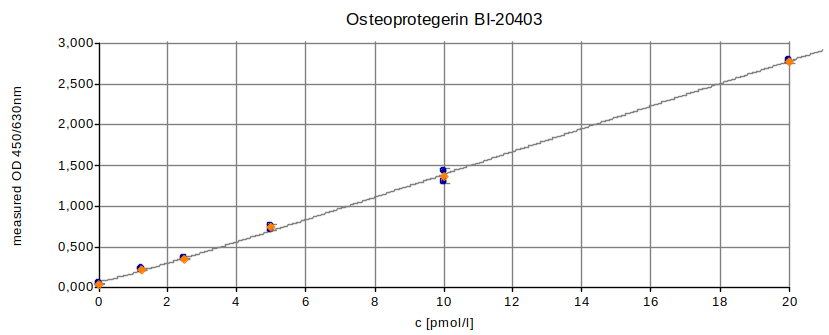
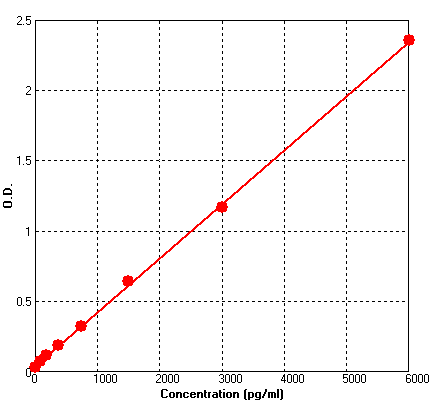
Human OPG PicoKine ELISA Kit standard curve
Human OPG (TNFRSF11B) / Osteoprotegerin ELISA Kit PicoKine(r)
EK0480
ReactivityHuman
Product group Assays
Overview
- SupplierBoster Bio
- Product NameHuman OPG (TNFRSF11B) / Osteoprotegerin ELISA Kit PicoKine(r)
- Delivery Days Customer9
- ApplicationsELISA
- Applications SupplierELI
- Assay Detection Range93.7 pg/ml - 6,000 pg/ml
- Assay Sensitivity<5 pg/ml
- Assay Time15-20
- CertificationResearch Use Only
- Scientific DescriptionHuman OPG (TNFRSF11B) / Osteoprotegerin ELISA Kit PicoKine® (96 Tests). Quantitate Human TNFRSF11B in cell culture supernatants, serum, plasma (heparin, EDTA) , saliva and urine. Sensitivity: 5pg/ml. The brand Picokine indicates this is a premium quality ELISA kit. Each Picokine kit delivers precise quantification, high sensitivity, and excellent reproducibility. Only our most reliable and effective kits qualify as Picokine, guaranteeing top-tier results for your assays.
- ReactivityHuman
- Reactivity SupplierHuman OPG
- Storage Instruction-20°C,2°C to 8°C
- UNSPSC41116158
References
- Zhang D, Xu C, Zhang J, et al. Plasma TNFRSF11B as a New Predictive Inflammatory Marker of Sepsis-ARDS with Endothelial Dysfunction. J Proteome Res. 2023,22(11):3640-3651. doi: 10.1021/acs.jproteome.3c00576Read this paper
- Elshamy AM, Hafez YM, Safa MAE, et al. The role of miR-433-3p in vascular calcification in type 2 diabetic patients: targeting WNT/β-Catenin and RANKL/RANK/OPG signaling pathways. Mol Biol Rep. 2023,50(11):9073-9083. doi: 10.1007/s11033-023-08792-9Read this paper
- Li Y, Yang S. Rb1 negatively regulates bone formation and remodeling through inhibiting transcriptional regulation of YAP in Glut1 and OPG expression and glucose metabolism in male mice. Mol Metab. 2022,66:101630. doi: 10.1016/j.molmet.2022.101630Read this paper
- Pingali U, Nutalapati C. Shilajit extract reduces oxidative stress, inflammation, and bone loss to dose-dependently preserve bone mineral density in postmenopausal women with osteopenia: A randomized, double-blind, placebo-controlled trial. Phytomedicine. 2022,105:154334. doi: 10.1016/j.phymed.2022.154334Read this paper
- Ma W, Jin W, He X, et al. Mycobacterium tuberculosis Induced Osteoblast Dysregulation Involved in Bone Destruction in Spinal Tuberculosis. Front Cell Infect Microbiol. 2022,12:780272. doi: 10.3389/fcimb.2022.780272Read this paper
- Bozkurt Doğan Ş, Öngöz Dede F, Ballı U, et al. Emerging roles of Interleukin-34 together with receptor activator of nuclear factor-kB ligand and osteoprotegerin levels in periodontal disease. Cytokine. 2021,144:155584. doi: 10.1016/j.cyto.2021.155584Read this paper
- Bonaccorsi G, Trentini A, Greco P, et al. Changes in Adipose Tissue Distribution and Association between Uric Acid and Bone Health during Menopause Transition. Int J Mol Sci. 2019,20(24). doi: 10.3390/ijms20246321Read this paper
- Liu S, Luo ZH, Ji GM, et al. Cajanolactone A from Cajanus cajan Promoted Osteoblast Differentiation in Human Bone Marrow Mesenchymal Stem Cells via Stimulating Wnt/LRP5/β-Catenin Signaling. Molecules. 2019,24(2). doi: 10.3390/molecules24020271Read this paper
- Huang YZ, He SK, Guo ZJ, et al. Nanostructured titanium surfaces fabricated by hydrothermal method: Influence of alkali conditions on the osteogenic performance of implants. Mater Sci Eng C Mater Biol Appl. 2019,94:1-10. doi: 10.1016/j.msec.2018.08.069Read this paper
- Zhang Q, Chen S, Shi J, et al. Coupled OPG-Fc on Decellularized Aortic Valves by EDC/NHS Attenuates Rat MSCs Calcification In Vitro. ASAIO J. 2019,65(2):197-204. doi: 10.1097/MAT.0000000000000796Read this paper